Field Story
Ten must see global nutrition stories from 2023
December 18, 2023
Better births in Bangladesh
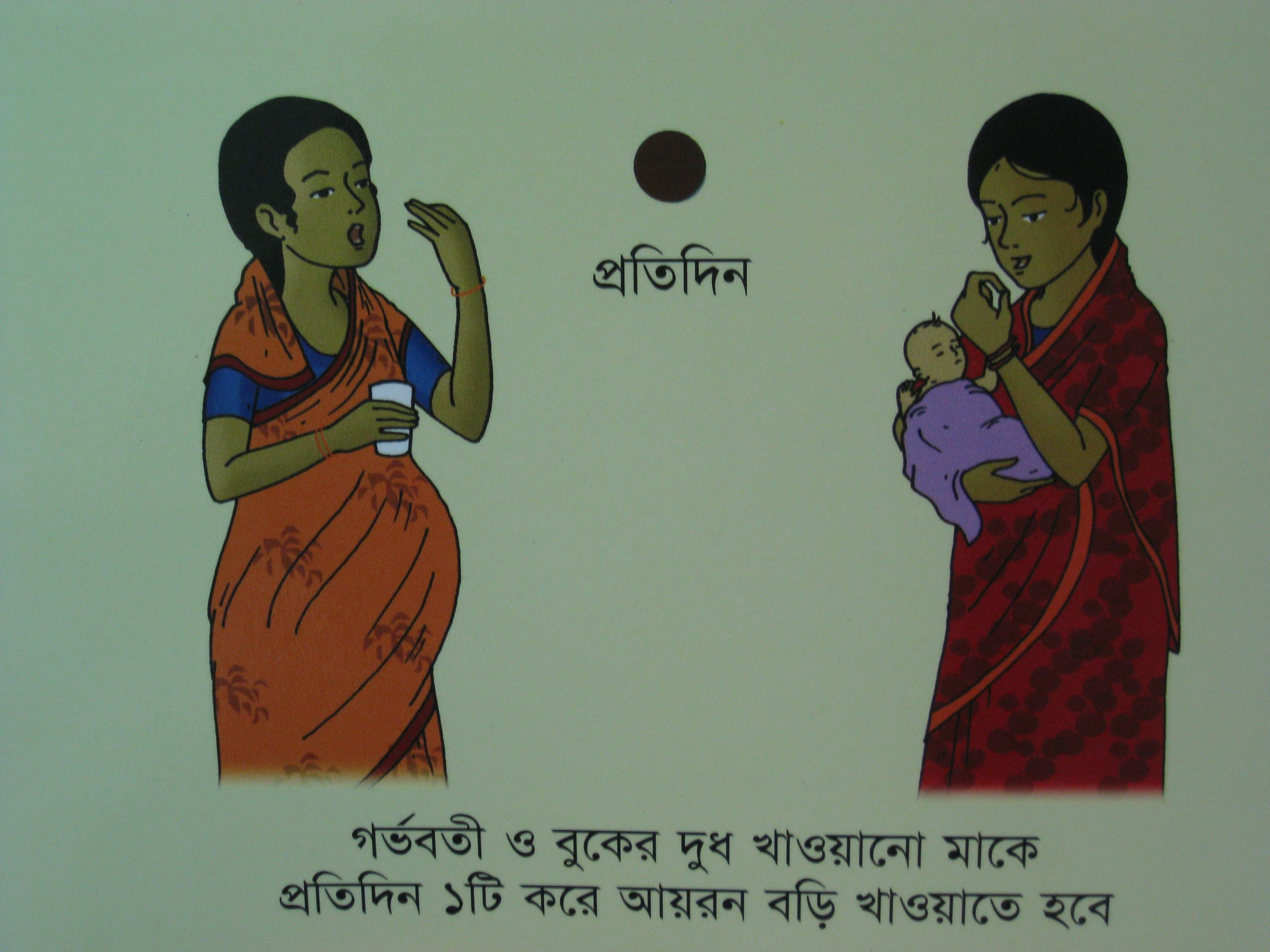
We know one of the best ways to keep women healthy during pregnancy. When women receive daily iron and folic acid (IFA) supplements as early as possible during pregnancy for at least 90 days, the results are multiplied for her and her newborn. It helps reduce anaemia and provides newborns a better chance at life.
Posted on May 29, 2015


We know one of the best ways to keep women healthy during pregnancy. When women receive daily iron and folic acid (IFA) supplements as early as possible during pregnancy for at least 90 days, the results are multiplied for her and her newborn.
It helps reduce anaemia and provides newborns a better chance at life. It’s low-cost, about 80 cents for a full 90-day supply, and extremely effective.
Seems simple, doesn’t it? And yet in many countries, supplementation levels for women are woefully low.
It’s standard practice in many countries to take regular iron and folic acid during pregnancy, but millions of women around the world still can’t access them early enough or often enough with other health services.
There are several interconnected reasons why women may not take the supplements. For one thing, the side effects of taking IFA can be pretty unpleasant, such as a burning sensation and constipation. A lack of supportive services, confusing messages and weak supply chain management for the supplements also leave women without access to this simple, low-cost intervention.
These obstacles can and are being overcome. A pilot project in Bangladesh saw a dramatic increase in the number of women taking IFA supplements by tackling some of these issues head on.
With funding from the Government of Canada through the Department of Foreign Affairs, Trade and Development, the Micronutrient Initiative partnered with the Government of Bangladesh and Institute of Public Health Nutrition to provide better services to pregnant women.
The project showed that anaemia could be reduced in pregnant women if they were provided with proper counselling on consuming IFA tablets, were given access to trained health staff and community workers, and had adequate supplies.
In Satkhira and Narsingdhi districts, we saw the percentage of women taking IFA supplements increase from about 51% to 98%; what’s more, the majority of these women took the full 90-day supply.
At the end of the project, seven out of ten women remembered how to mitigate side-effects and this high level of knowledge was found to be directly linked to efficient and consistent counselling by frontline workers during ante-natal care at clinics and during home visits.
We’re using this pilot project to help revive the interest in IFA programs for pregnant women in Bangladesh, giving the government strong evidence to strengthen its programs.
 Since the government was part of the study throughout, it feels a strong sense of ownership over the results.
Since the government was part of the study throughout, it feels a strong sense of ownership over the results.
It’s working on supply chain management to ensure supplements are available to women and has committed to using the same model in ten more districts in the country where IFA coverage among pregnant women is low.
This will revive a health program that seemed to be floundering, it will recharge efforts in the country to ensure the mothers of Bangladesh are well cared for and their newborns are born stronger and with a better chance at life.
I hope that other countries will take notice of these results, too, and share them across the region and around the world.
The Canadian Network for Maternal, Newborn and Child Health partner organizations and institutions that are on the front lines can also use this evidence to inform their own programs as part of our collective exchange of knowledge.
The evidence is there about what works – and what we need to do more of to save and improve lives.
Projects like this one in Bangladesh show us what’s possible when we put women first, equip them with the right knowledge, and give them what they need for healthy pregnancies and healthy births.
This piece was originally published on the Canadian Network for Maternal, Newborn Child Health Blog on 05/28/2015.