News
Canada announces historic investment in the global fight against malnutrition
February 6, 2025
WP_Term Object
(
[term_id] => 49
[name] => Field Stories
[slug] => all-field-stories
[term_group] => 0
[term_taxonomy_id] => 49
[taxonomy] => news-category
[description] => Discover the personal stories of people whose lives have been impacted by better nutrition, and those working tirelessly to deliver it.
[parent] => 0
[count] => 180
[filter] => raw
)
Lady health workers are a key link to successful breastfeeding in Pakistan
For World Breastfeeding Week, we’re celebrating front line health workers in Pakistan who combat misconceptions, create awareness and provide skilled breastfeeding support to rural communities. Read about the difference they’re making for families.
Posted on July 29, 2021
When Nutrition International embarked on the Right Start program in Pakistan – an initiative to provide pregnant women, newborns and young children with better nutrition and healthcare – program designers recognized the need to tap into the women-led healthcare contingent that had established relationships at the community level: lady health workers and community midwives.
The importance of breastfeeding was a core component of the trainings, which focused on maternal and child health best practices for the first 1,000 days – a critical growth window from the time of conception until two years.
Nutrition International, working closely with the Department of Health, facilitated the trainings for front-line health workers at the community level. Enhancing interpersonal communication skills to provide improved counselling and skilled lactation support were central training elements. The goal? To equip families with knowledge on the power of breastfeeding and mothers with the skills to successfully breastfeed their newborns to build immunity and support optimal growth. Myths, fears and misconceptions that threatened the success of breastfeeding were also carefully discussed and evidence-based advice was provided to help dispel these risks.
That skilled counselling is seeing results.
“Lady health workers are able to change perception to encourage family support,” said Dr. Sarwan Kumar, Nutrition International’s Project Coordinator in Sindh, who has been part of the initiative since 2017. “Sufficient breastfeeding will come when society, when family members, provide an enabling environment for the mother to adopt this practice. Women might have an idea to breastfeed, but they might not get the family support and might not be aware of the importance of breastfeeding.”
“Sufficient breastfeeding will come when society, when family members, provide an enabling environment for the mother to adopt this practice.” – Dr. Sarwan Kumar, Nutrition International Project Coordinator, Sindh, Pakistan
In addition to door-to-door visits, lady health workers hosted peer sessions where pregnant women and lactating mothers attended alongside their family members. Community midwives incorporated counselling into pre- and post-natal check-ups. To accommodate for COVID-19 safety regulations, the meeting size for peer support groups was reduced, and strict protocols for face coverings and handwashing were put in place. In addition, Nutrition International supplied PPE, such as masks and hand sanitizer, so health workers could safely continue their work, which became even more critical as fears around COVID-19 increased hesitancy for families to access healthcare.
Below we look at three examples where front-line health workers’ instrumental support has facilitated positive behaviour change. At its core is promoting breastfeeding by giving mothers and their families the information they need to make informed decisions and the skills to successfully breastfeed.
Location: Jamshoro, Sindh
The challenge: Myths and misconceptions related to safe motherhood practices are common in Ashok Kumar and Shano’s village in Jamshoro district, Sindh. Mothers in the area often believe that colostrum, the initial breast milk that is a yellowish colour, is harmful for their newborn. Instead, a newborn is given goat’s milk, which not only can be difficult on digestion, but causes a newborn to miss out on the important immunity building benefits of colostrum.
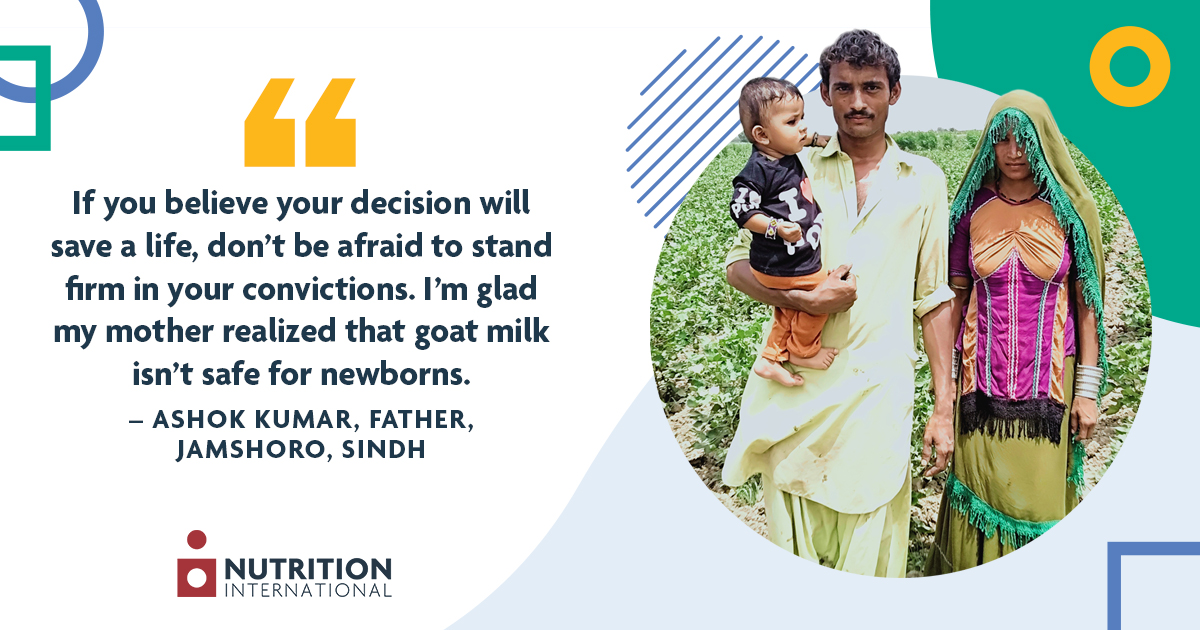
What happened: While pregnant, Shano, supported by her husband Ashok, attended awareness sessions held by the lady health worker and community midwife in her area. She learned what was meant by the first 1,000 days, the benefits of initiating breastfeeding within one hour of birth, exclusive breastfeeding for the first six months, and the introduction of complementary foods from six months, and continued breastfeeding for two years and beyond. She wanted to adopt the practices as advised and diligently followed all prenatal instructions she was given.
Shano gave birth at her community midwife’s birthing station. Under her midwife’s instruction, she started breastfeeding soon after Ramesh was born. Shano was discharged with her baby after the community midwife held a counselling session with both Shano and her husband on exclusive breastfeeding for the first six months.
However, soon after returning home, Shano’s mother-in-law gave Ramesh goat milk. He developed a gastric problem and the family returned to the clinic. Upon examination, the midwife asked whether animal milk had been given to their baby, despite counselling. Shano’s husband, Ashok, confirmed what happened. “It is difficult to break down cultural barriers,” Ashok explained. After leaving the clinic, they were able to speak to his mom and explain to her why exclusive breastfeeding until six months would be the best thing for her grandson. “If you believe your decision will save a life, don’t be afraid to stand firm in your convictions. I’m glad my mother realized that goat milk isn’t safe for newborns.”
A farm labourer, Shano carries her now 11-month-old son with her when she goes to the field so she can continue to breastfeed him. She introduced complementary foods at six months and plans to continue to breastfeed until at least two years. “I make every effort to breastfeed my son whenever possible,” she shared. “I want my son to be strong and intelligent.”
Location: Khairpur, Sindh
The challenge: When Hamza was born, his mother, Sobia, started feeding him cow’s milk within the first few days of his life. Sobia assumed her breastmilk would not be enough to meet the dietary requirements of her growing boy. She also found the bottle easier, as she felt tired after breastfeeding and Hamza would still be hungry even after long breastfeeding sessions.
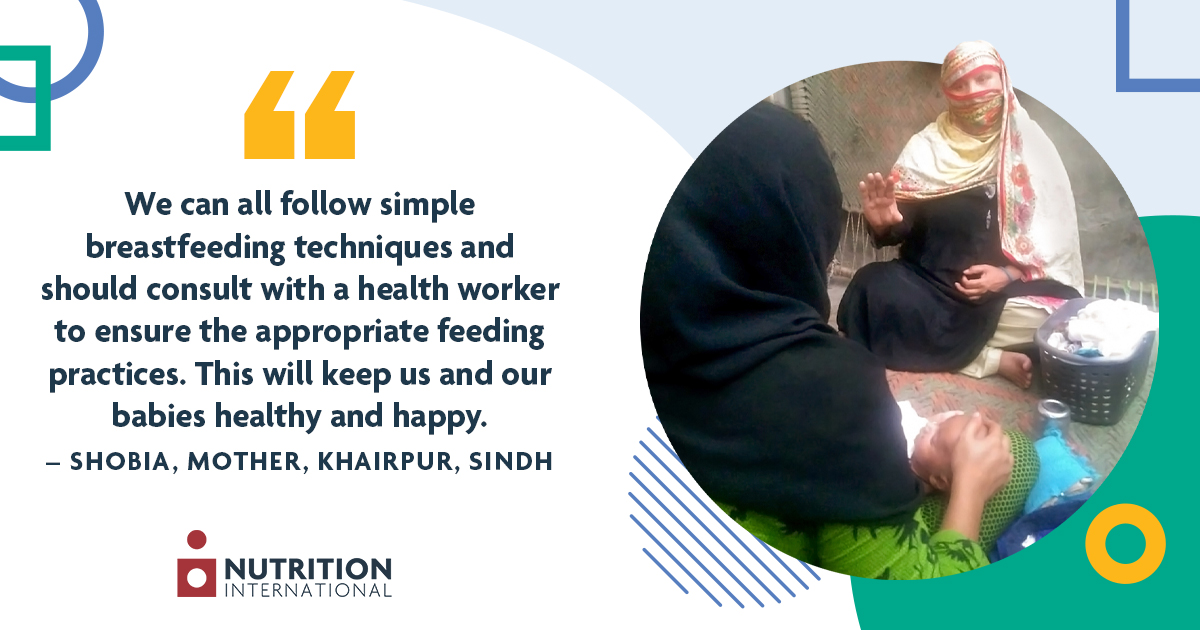
What happened: During a door-to-door visit from Rani Ansari, a lady health worker in the community, Sobia shared that her newborn often had bouts of diarrhea, and she was worried because he seemed weak and was constantly crying. As they continued speaking together, Sobia also shared that she was only breastfeeding two to three time a day because she didn’t have enough milk.
Rani asked to observe her breastfeeding to see if she could offer any helpful advice. She noticed a challenge with the positioning and latching which could impact Hamza’s ability to get enough milk while feeding. Taking her time, Rani suggested alternative ways for Sobia to hold her baby while breastfeeding in order to help her child get more milk in the same amount of time. She also reassured Sobia and encouraged her to try out the new method and see if she noticed any positive changes. Further, she advised that diarrhea can be caused by giving cow’s milk, which is difficult for a newborn to digest, as well as by the bottle it was being given in, if it wasn’t being hygienically cleaned and washed.
After a few more counselling sessions, and actively supporting new positioning, Sobia said she started to notice a difference. Within a week, her child’s physical appearance improved, he stopped having diarrhea when she stopped giving him cow’s milk, and she herself started feeling more comfortable and confident. Additionally, Hamza started sleeping peacefully after a breastfeeding session.
“I am feeling more comfortable with my body and relaxed most of the times,” Sobia shared. “Now, I am feeding my child on demand, at least 10 to 12 times in 24-hours. I am happy that by following these simple steps, I can save money which I was spending to travel to the doctor and on medicines. We can all follow simple breastfeeding techniques and should consult with a health worker to ensure the appropriate feeding practices. This will keep us and our babies healthy and happy.”
Location: Swabi, Khyber Pakhtunkhwa
The challenge: Traditional communities living in Swabi district are known for hospitality and rich cultural values. There can also be strict rules, regulations and restrictions placed on women. Due to this, women and caregivers are often not aware of the recommended best practices for breastfeeding. Myths exist that affect maternal and neonatal health, but since reproductive health is a sensitive issue, it can be a challenge for a health worker to share information at the community level.

What happened: Through close collaboration and with the support of government health programs, lady health workers were able to find opportunities to share maternal health and breastfeeding best practices with women who were looking for more information in relation to themselves and caring for their babies.
Ansar Bibi, a lady health worker in the area, was given a target of 50 beneficiaries to counsel. She said she felt properly prepared for the job. “I was very well oriented by our lady health supervisor about key messages on breastfeeding,” Ansar said. She also utilized PPE and followed COVID-19 safety protocols, as the pandemic caused a further layer of hesitation for households. “I am thankful to Nutrition International for poster provisions along with face masks and hand sanitizers for safe community access.”
One of the mothers Ansar met with was Azra Aamir, who was having difficulty with milk production and positioning her baby while breastfeeding. “I had little knowledge about early initiation and exclusive breastfeeding. Even though I am educated, I had a lack of awareness about proper positioning and techniques during breastfeeding,” Azra said. By gaining exposure, she was able to remedy the issues she was having. “I am thankful to the lady health worker, the health department and Nutrition International for educating mothers like me.”
Front line health workers have reached 50,000 pregnant and lactating women and caregivers in Swabi district through this targeted, thoughtful approach that ensures maternal health information is available and women have the support they need to breastfeed.